|
In 2016, a taskforce by the Society of Critical Care Medicine and the European Society of Intensive Care Medicine proposed new criteria to define sepsis: the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). They unanimously agreed that the original SIRS criteria to be unhelpful.
Recommendations
| Sepsis-3 | 1991 Sepsis Consensus |
|---|
| Definition of Sepsis | Sepsis is life-threatening organ dysfunction caused by a dysregulated host response to infection.
Clinical criteria: acute change in SOFA (Sepsis-related Organ Failure Assessment) score ≥2 points consequent to the infection (see below for scoring) | Sepsis is SIRS (Systemic Inflammatory Response Syndrome) with a source of infection. SIRS is ≥2 of: • Temperature >38C or <36C • Heart rate >90/min • Respiratory rate >20/min or PaCO2 <32 mmHg (4.3 kPa) • White blood cell count >12000/mm3 or <4000/mm3
Severe sepsis is sepsis complicated by organ dysfunction.
| | Definition of Septic Shock | Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality.
Clinical criteria: hypotension requiring use of vasopressors to maintain mean blood pressure of ≥65 mmHg, and having a serum lactate level >2 mmol/L persisting after adequate fluid resuscitation.
| Septic shock is sepsis-induced hypotension persisting despite adequate fluid resuscitation.
| | Screening | | qSOFA (to identify patients with suspected infection who are likely to have a prolonged ICU stay or to die in hospital) is ≥2 of: • Alteration in mental status (GCS ≤13) • SBP ≤100mmHg • Respiratory rate ≥22/min | Above |
SOFA score
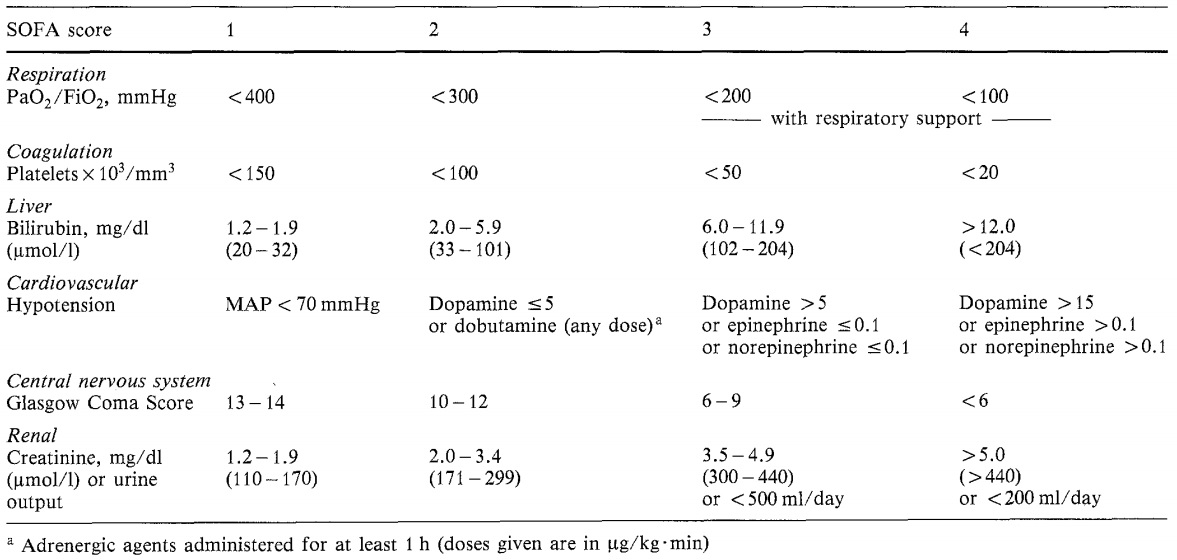
Image from Vincent et al Baseline SOFA score can be assumed to be zero in patients not known to have pre-existing organ dysfunction.
Clinical features in the septic patient:
- Tachycardia, tachypnea, raised WCC and inflammatory markers, pyrexia/hypothermia
- Symptoms and signs related to the organ system affected infection: - UTI: pain, foul smelling dark urine etc - Chest: SOB, low saturations, cough - Wound infection: discharge, pain, dehiscence
- Clammy
- Warm peripheries (The latter is a distinct feature from other types of shock where peripheral vasoconstriction leads to cold peripheries. Whereas in sepsis vasodilatation due to bacterial toxins leads to warm peripheries. This in turn leads to reduced venous return, preload and reduced cardiac output leading to low blood pressure in severe sepsis and septic shock) Metabolic acidosis, raised lactate Hypotension and reduced urine output
Management
Based on parameters above establish how unwell the patient is.
- IV access, bloods, blood cultures, venous blood gas/arterial blood gas
- Fluids (establish pre-resus fluid status clinically, i.e. check JVP, pitting oedema, crepts in the chest, mucus membranes, skin turgor, check fluid balance chart if available, check recent CXR, ECHOS, patients medication)
- Choice of fluid: In sepsis crystalloid (normal saline Hartmann's) or colloid may be used.
- Catheterisation: If patient unable to move, has severe sepsis, low urine output, deranged U&Es consider catheterisation inorder to enable more intensive monitoring.
- Culture everything: blood, urine, sputum, wound swabs
- Routine investigations - CXR, ECG - Antibiotics: Choice dependent on most likely presumed source. Use local protocols and guidelines when choosing antibiotics and check recent microbiology results/organisms grown and sensitivity profiles.
- Regular observations
- Critical care outreach input or a more formal ITU review should be requested if condition deteriorating or in septic shock. In patients with comorbidities especially those with cardiac problems who require close fluid status monitoring will benefit from early intensive care input where appropriate.
References
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:801?10.doi:10.1001/jama.2016.0287
Vincent JL, Moreno R, Takala J, et al; Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707-710.
Author:
Mr Kasun Wanigasooriya MBCHB, MRCS
| Speciality:
General Surgery
| Date Added:
02/07/2011
|