|
Useful background information
Patient information/counselling
Anticoagulation guidelines
Sedation guidelines
Procedure
in accordance with BSG/AUGIS quality statement 2017
- Standardised anatomical landmarks in a complete OGD: Procedure should start at the upper oesophageal sphincter and reach the second part of the duodenum, to include the upper oesophagus, gastro-oesophageal junction, fundus, gastric body, incisura, antrum, duodenal bulb and distal duodenum. The fundus should be inspected by a J-manoeuvre in all patients, and where there is a hiatus hernia the diaphragmatic pinch should be inspected while in retroflexion, and size and integrity of the oesophago-gastric junction assessed.
- Photo-documentation of relevant landmarks and any detected lesions (see ESGE guidelines with eight anatomical landmarks)
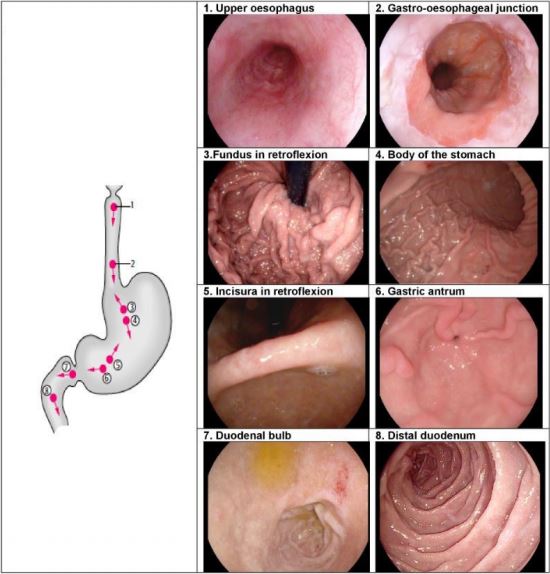
Image from Synder et al
- Inspection (during withdrawal) of OGD should take an average of 7 mins. Total inspection time for high-risk and surveillance procedures should be recorded.
- Paris classification should be used to describe lesions detected (including those within Barrett's segment) and targeted biopsies taken.
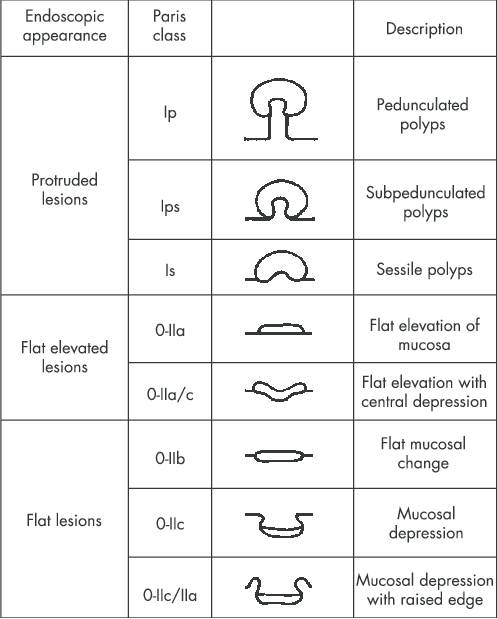
Image from Hurlstone et al
- Prague classification should be used to describe Barrett's oesophagus.
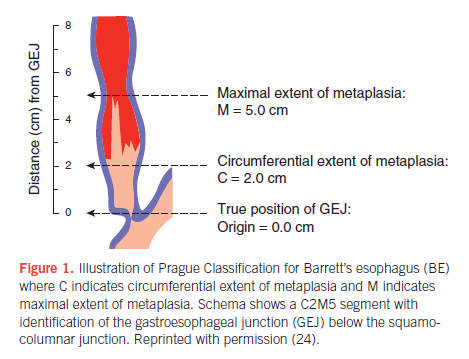
Image from Shaheen et al
An excellent article detailing each step of the upper GI endoscopy procedure can be found here
Management of lesions detected on endoscopy
- If no lesions detected within Barrett's segment: Take biopsies according to Seattle protocol (quadrantic biopsy specimens taken at 2 cm intervals).
- Suspected squamous neoplasia: Full assessment with enhanced imaging and/or Lugol's chromo-endoscopy.
- Oesophageal ulcers and oesophagitis that is grade D or atypical in appearance: Take biopsy and further evaluate in 6 weeks after proton pump inhibitor therapy.
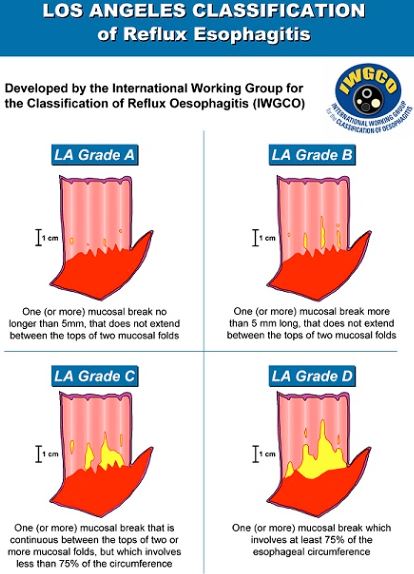
Source: International Working Group for the Classification of Oesophagitis
- Varices: Classify according to size (Grade 1-3)
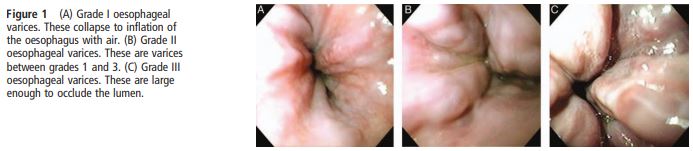
Image from Tripathi et al
- Gastric or duodenal ulcers: H. pylori should be tested and eradicated if positive. Additionally for gastric ulcers, biopsy and re-evaluate after appropriate treatment (e.g. H. pylori eradication where indicated) within 6-8weeks.
- Endoscopic features of gastric atrophy or intestinal metaplasia: Take separate biopsies from the gastric antrum and body.
- Gastric polyps: Document presence, number, size, location and morphology, and take biopsies.
- Malignant looking lesion: Photo-document and take a minimum of six biopsies
- Suspected coeliac disease: Take a minimum of four biopsies, including representative biopsies from the second part of the duodenum and at least one from the duodenal bulb
- Where iron deficiency anaemia is being investigated: Take separate biopsies from the gastric antrum and body, as well as duodenal biopsies if coeliac serology is positive or has not been previously measured.
- For patients with dysphagia/food bolus obstruction with no cause found: Take biopsies from two different regions in the oesophagus to rule out eosinophilic oesophagitis.
References
Beg S, Ragunath K, Wyman A, et al. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut 2017;66:1886-1899.
Lee SH, Park YK, Cho SM, et al.Technical skills and training of upper gastrointestinal endoscopy for new beginners. World J Gastroenterol. 2015 Jan 21; 21(3): 759-785. doi: 10.3748/wjg.v21.i3.759
Snyder CW, Vandromme MJ, Tyra SL, et al. Retention of colonoscopy skills after virtual reality simulator training by independent and proctored methods. Am Surg 2010;76:743-6.
Hurlstone D, Sanders D, Atkinson R, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: Can we change the endoscopic management paradigm?. Gut 2007;56:838-46. doi:10.1136/gut.2006.106294.
Shaheen N, Falk G, Iyer P, Gerson L. ACG Clinical Guideline: Diagnosis and Management of Barrett's Esophagus. American Journal of Gastroenterology 2016;111:30-50. doi: 10.1038/ajg.2015.322.
Tripathi D, Stanley AJ, Hayes PC, et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 2015;64:1680-1704.
Further Reading on Colonoscopy
Patient information
Anticoagulation guidelines
Sedation guidelines
Bowel preparation guidelines
Surveillance guidelines
Author:
Ms Yanyu Tan
| Speciality:
Surgical Procedures
| Date Added:
12/11/2019
|